Controlling Cervical Cancer: DCEG’s Ongoing Commitment to Improving Women’s Health
, by Jennifer K. Loukissas, M.P.P.
Scientists in DCEG are among the leaders of a growing global effort to greatly reduce the number of deaths each year from cervical cancer. They are building upon a legacy of research advances on this malignancy, sprouting from decades of investment in natural history studies. By leveraging support from the Cancer MoonshotSM, partnerships with non-profits, integrated health care systems, pharmaceutical and medical research companies, and others, DCEG investigators have launched a multi-faceted, highly-integrated research program to improve both primary and secondary prevention for a malignancy that affects more than half a million women each year and causes over 300,000 deaths worldwide.
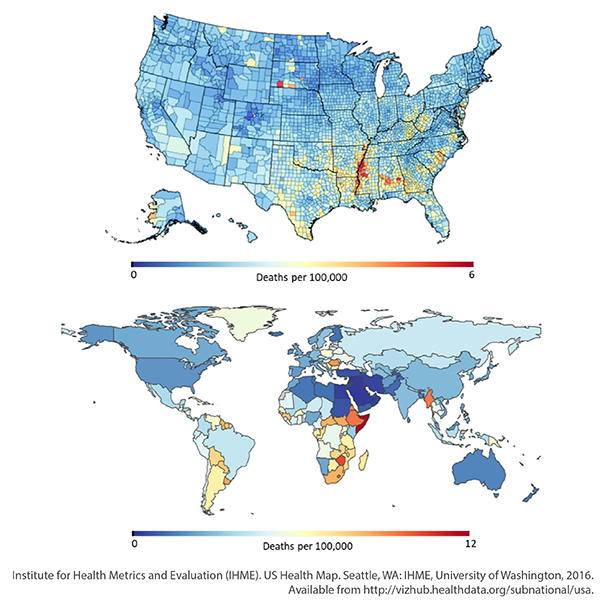
Cervical cancer is a sentinel malignancy of health disparities: women of means, with routine access to accurate screening—which can identify and remove precancerous lesions—rarely develop the cancer, and even less frequently die from it. Women of lesser means are less frequently vaccinated, screened, and treated, particularly at the precancerous stage. The disparities are related to resources, not countries. For example, women in Mississippi have nearly double the risk of developing or dying from cervical cancer compared to women living in Vermont. The incidence rates in the period 2011 through 2015 for these two states were 9.5 and 4.4 cases per 100,000 women, respectively, while mortality rates were 3.5 and 1.0 deaths per 100,000 women (data from the Centers for Disease Control and Prevention).
Knowing the natural history allows for rigorous refinement of prevention methods
The steps leading to cervical carcinogenesis—infection with human papillomavirus (HPV), persistence and progression to precancer, and invasion—are universal. Although prophylactic vaccines are currently available, cervical cancer can still arise among women already infected with HPV before the vaccine era. Control efforts based solely on vaccination of adolescents would take another 40+ years. Improved screening and diagnosis of screen-positive women can accelerate control by decades. These efforts are particularly important because deaths from cervical cancer are rising as the global population ages.
Research on such secondary prevention efforts is being led by Mark Schiffman, M.D., M.P.H., senior investigator in the Clinical Genetics Branch (CGB), and Nicolas Wentzensen, M.D., Ph.D., M.S., senior investigator, Deputy Chief of CGB, and chief of the Clinical Epidemiology Unit, with a team comprising staff scientists, postdoctoral fellows, predoctoral fellows, and special volunteers.
With critical support from the Cancer Moonshot, the Cervical Cancer Control and HPV Vaccine Trial projects will capitalize on the breadth and depth of etiologic and laboratory research to refine and validate optimal cervical screening methods and clinical management strategies for both high- and low-resource settings.
The team takes a comprehensive approach to the development of screening technologies. Cost-effectiveness is especially important for low- and middle-income settings (LMIs), where resource limitations have meant that fewer than five percent of eligible girls have been vaccinated, and high-quality cervical cancer screening modalities are too time-intensive and expensive for routine use (Wentzensen N, Schiffman M. Accelerating cervical cancer control. Lancet Public Health 2018).
In low-resource settings, including regions of the U.S., the costs and complexities of approved and commercially available HPV screening tests remain excessive, resulting in very little uptake. In high-resource settings, there is debate over which of the new, HPV-based test methods to adopt, and how to combine them with triage tests to reduce overtreatment. Uneven access to new methods increases cervical cancer health disparities, with inadequate screening in low-resource settings and overtreatment in high-resource regions.
Primary prevention with one shot: proving efficacy of one dose of the HPV vaccine
Investigators in the Infections and Immunoepidemiology Branch (IIB) conducted the first federally-funded clinical trial of the HPV vaccine in Costa Rica in the early 2000s. “The development of the prophylactic HPV vaccine revolutionized the future of cervical cancer prevention,” said Aimée Kreimer, Ph.D., senior investigator in IIB. “Yet, the cost and spacing requirements of the three-dose regimen kept it out of reach for women living in low-resource settings who could benefit from it the most.”
When initially licensed, the vaccine was approved in a three-dose regimen spaced over a six-month period. Based on immunogenicity trial results showing comparable immune responses with two and three doses and evidence for efficacy after two doses from the original Costa Rica Trial, the recommendations were changed to just two doses for adolescents. “Formal analyses from immunogenicity trials showed that teens who received two doses mounted an equivalent or even better immune response than adult women who received three doses and a post-hoc analysis of our data from Costa Rica showed that two doses provided strong protection against HPV infections caused by the types included in the vaccine,” she explained.
Data from the Costa Rica Trial also generated the first evidence that even a single dose of bivalent vaccine provides protection against infection and generates vaccine-induced stable antibody titers. The latest data, which are under review, suggest a decade or more of protection, following initial vaccination, irrespective of number of doses received.
However, to change recommendations from a multi-dose regimen to one-dose, organizations like the U.S. Food and Drug Administration, the European Medicines Agency, and other governing bodies require data from formal randomized trials designed to test the efficacy of a single dose, not just post-hoc analyses of the three-dose trial. To provide that evidence, Dr. Kreimer and Allan Hildesheim, Ph.D., senior investigator in IIB, and Joshua Sampson, Ph.D., senior investigator in the Biostatistics Branch, working in collaboration with investigators at Agencia Costarricense de Investigaciones Biomédicas (the Agency for Biomedical Research in Costa Rica), the World Health Organization’s International Agency for Research on Cancer, and in partnership with the Bill and Melinda Gates Foundation, launched a formal, prospective evaluation of one and two doses of the bivalent and nonavalent vaccines in a non-inferiority randomized clinical trial among 20,000 adolescents in Costa Rica. “In addition to the randomized component, designed to show non-inferiority of one compared to two doses, this study plans to enroll 4,000 young adult women into an epidemiological survey to quantify the degree of efficacy of a single-dose regimen,” said Dr. Kreimer. “If successful, results from our trial will provide the evidence to support single-dose guidelines for the vaccine, allowing the existing store of vaccine to go further while reducing the cost of vaccination overall.”
Improved screening could accelerate control by decades
While the promise of the vaccine is alluring, millions of women already exposed to HPV are at risk for cervical cancer. “There will be a day, perhaps 25-30 years from now, when we see a profound decline in cervical cancer mortality in low- and middle-resource settings due to vaccination,” said Dr. Schiffman. “In the meantime, women living in those circumstances need screening protocols to address prevalent precancer and make an immediate impact on the number of deaths each year. We are testing easy and inexpensive screening that can be paired with on-the-spot treatment of women with worrisome cell changes.”
When health-care access is limited, or resources are scarce, intensive screening approaches are prohibitively expensive and logistically infeasible. Aside from the complex medical infrastructure required by contemporary approaches, screening today is incredibly time-intensive. Assay run-times are long, women must return for follow-up screening on initial results, and if treatment is necessary, that may mean a third visit, often at a different location.
To reduce wait times and staffing needs in clinics, self-sampling kits are being field-tested among women in Costa Rica, Brazil, and Nigeria.
Drs. Schiffman and Wentzensen are collaborating with foundations and industry groups to develop and validate rapid, inexpensive, point-of-care screening methods. Women identified as HPV-positive from a self-collected sample may go immediately to automated visual evaluation (AVE), a deep-learning, artificial intelligence algorithm developed in collaboration with Global Good, a fund at Intellectual Ventures, that eliminates the need for highly-trained experts to conduct colposcopy (visualization of the cervix, and biopsy of suspicious areas) as well as expensive and time-consuming pathology. In their analysis of the approach, AVE performed better than other tests, including a human expert, at identifying precancer (Hu L et al. An Observational Study of Deep Learning and Automated Evaluation of Cervical Images for Cancer Screening. JNCI 2019). Dr. Schiffman projected, “If we were able to screen all women in the target population of ages 25-49 just once, we could identify and treat 60 percent of the precancer or cancer expected to arise in the entire population.”
AVE will revolutionize cervical cancer screening in low-resource settings. In field studies currently underway or soon to start, a health worker, after minimal training, uses a speculum to visualize the cervix, swabs it with acetic acid—which turns cells white if they have HPV infection, inflammation, precancer or cancer—and then takes a picture with a cell phone camera loaded with the AVE algorithm. The image is processed with the algorithm and immediately, a result is produced. Women may be identified as having a healthy/normal cervix, abnormal (apparent cell changes that are likely to go on to become precancer) precancer, or cancer.
If AVE produces a result of low-or no risk, the likelihood that this woman will develop cervical cancer in the coming years is low. If she is at risk, she can immediately be treated with cryotherapy (freezing off the worrisome cells) or burning/cauterizing. These treatments are fast, out-patient, and can be provided on the same day as the screening, in the same facility.
Other triage strategies for high- and low-resource settings
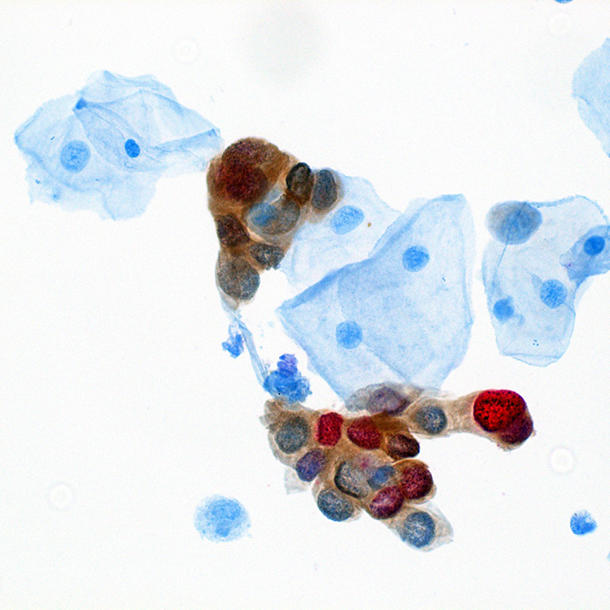
The CGB team is working on several other screening and triage approaches for high- and low-resource settings. Dr. Wentzensen, postdoctoral fellow Megan Clarke, Ph.D., and colleagues evaluated a dual-stain laboratory test that measures the presence of two proteins, p16 and Ki-67, associated with HPV-caused precancers, on cervical cytology slides. Dual-stain testing more accurately predicted five-year risk of cervical precancer for HPV-positive women, compared to cytology (Clarke MA et al. Five-Year Risk of Cervical Precancer Following p16/Ki-67 Dual-Stain Triage of HPV-Positive Women. JAMA Oncology 2018). In a subsequent study, dual stain was shown to be more efficient than the currently approved triage strategy in the U.S., cytology and HPV genotyping (Wentzensen N et al. JAMA Internal Medicine, in press). The Cancer Moonshot is now supporting efforts to develop an automated evaluation of dual stain slides using machine learning approaches.
Another approach, developed by the same team along with laboratory colleagues in the Cancer Genomics Research Laboratory and elsewhere, looks for HPV methylation in 12 high-risk types to determine risk of a positive HPV screening test result. Compared with cytology, HPV methylation testing has greater accuracy for detecting cervical precancer, with lower colposcopy referral rates, and demonstrates clinically useful risk stratification for cervical precancer beyond HPV genotyping information alone (Clarke et al. Human papillomavirus DNA methylation as a biomarker for cervical precancer: Consistency across 12 genotypes and potential impact on management of HPV-positive women. Clin Cancer Res 2018). The HPV methylation test is now being evaluated in self-sampled specimens to make it an option for low-resource settings.
While routine screening in high-resource settings controls the majority of cervical precancer and cancer, women in such programs often undergo unnecessary follow-up procedures and overtreatment. Studies by Drs. Schiffman, Wentzensen, and others have shown that a minority of persistent infections go on to cause precancer. “We know so much about the way HPV operates at the cervix, we can avoid overtreatment and reduce harm and time spent in medical appointments, without sacrificing cancer prevention at the population level,” said Dr. Schiffman. The major focus would be on improving the accuracy, efficiency, and population reach of screening by switching to risk-based guidelines that emphasize objective tests (including HPV testing and biomarkers for triage).
“By the conclusion of these efforts, we will be ready to pair HPV vaccination with the best screening methods in widespread applications tailored to resources, to accelerate cancer control based on firm science and best practices,” said Dr. Wentzensen.