HPV Vaccine Protection Outweighs Additional Risk of Cervical Lesions Caused by Non-Preventable HPV Types
, by Maura Kate Costello, M.A.
The human papillomavirus (HPV) vaccine has provided tremendous protection against HPV infection and associated endpoints, like cervical precancer. However, the vaccine targets the most prevalent and carcinogenic HPV types, which may leave vaccinated individuals susceptible to lesions caused by the other types.
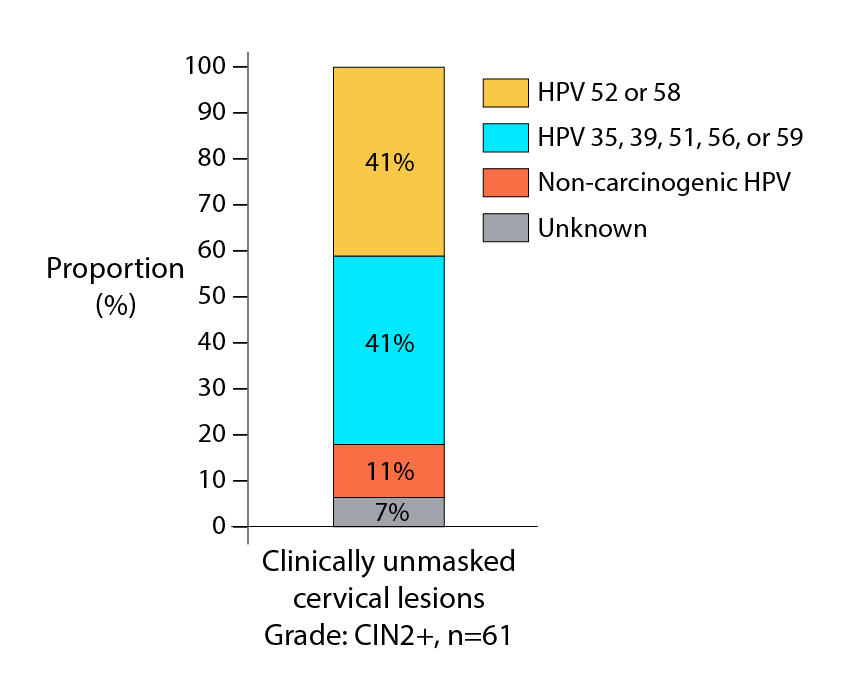
In a new study analyzing data from the publicly funded Costa Rica HPV Vaccine Trial (CVT), Jaimie Shing, Ph.D., M.P.H., postdoctoral fellow in the Infections and Immunoepidemiology Branch, and colleagues, found that the HPV types not targeted by the vaccine cause cervical lesions more frequently in vaccinated populations than in unvaccinated populations.
Since the HPV vaccine protects against the more carcinogenic HPV types, vaccinated individuals need clinical treatment, such as the loop electrosurgical excision procedure (LEEP) or laser ablation, less frequently than unvaccinated individuals. This reduction in clinical treatment creates the opportunity for slower growing types—those not targeted by the vaccine—to cause cervical lesions in vaccinated individuals in the long-term. This phenomenon is called clinical unmasking. Published in the journal, Lancet Oncology, on June 13, 2022, this study is the first to observe and evaluate clinical unmasking following HPV vaccination.
The investigators also estimated that, among vaccinated individuals, the overall number of cervical lesions the HPV vaccine was able to prevent was considerably greater than the number of additional, clinically unmasked lesions caused by non-preventable HPV types.
The results of this study emphasize the need for vaccinated individuals to continue regular screening so that non-preventable HPV types can be detected and treated prior to their progression to cervical cancer. Additionally, these findings confirm that the HPV vaccine is highly effective and essential for cervical cancer prevention.
Previous work in DCEG has shown that the HPV vaccine would prevent most cervical cancers across racial and ethnic groups.
Reference
Shing JZ, et al. Precancerous cervical lesions caused by non-vaccine-preventable HPV types after vaccination with the bivalent AS04-adjuvanted HPV vaccine: an analysis of the long-term follow-up study from the randomised Costa Rica HPV Vaccine Trial. Lancet Oncol. June 2022.