Testing for IBMFS Important for Treatment Decisions in Severe Aplastic Anemia
, by Jennifer K. Loukissas, M.P.P.
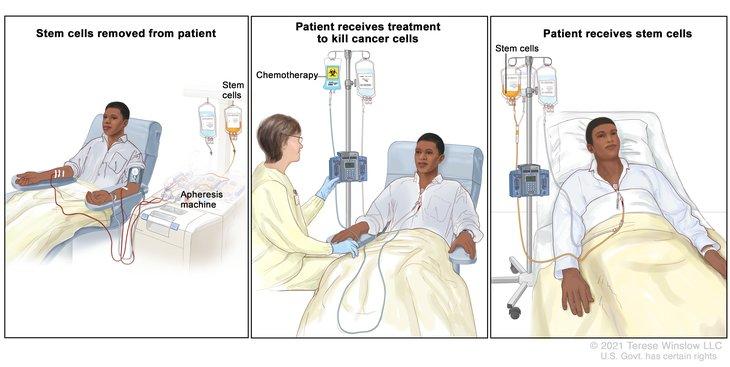
Individuals who receive hematopoietic cell transplant for treatment (HCT) of severe aplastic anemia (SAA) can benefit from genetic testing prior to treatment initiation to determine if they have an unrecognized inherited bone marrow failure syndrome (IBMFS) and therefore need disease-specific HCT regimens and follow-up plans, according to a new study published July 1, 2022, in the journal Blood.
SAA is a bone marrow failure disorder that can be caused by immune-mediated mechanisms or rare germline pathogenic variant(s). To increase the chances for successful outcomes in these patients, treatments including HCT must be customized to their underlying pathophysiology.
Lisa J. McReynolds, M.D., Ph.D., assistant clinical investigator, Maryam Rafati, M.D., Ph.D., geneticist, and colleagues, in the Clinical Genetics Branch, evaluated over 700 patients who underwent HCT for SAA in the NCI-CIBMTR Transplant Outcomes in Aplastic Anemia (TOAA) study. They identified patients with unrecognized IBMFS and carriers of pathogenic or likely pathogenic variants in IBMFS genes and evaluated the effect of variant status on HCT outcomes. They found that patients who had unrecognized IBMFS but received standard SAA treatment did worse than those with acquired SAA receiving the same treatment.
Most patients with IBMFS are identified in childhood when a clinical exam reveals phenotypic features, or by report of family history. However, there is growing recognition that these disorders can present without physical features and/or family history, leading to delayed or misdiagnosis, particularly in adults.
Learn more about the Clinical Genetics Branch research program on predictors of HCT outcomes.
Reference
McReynolds LJ et al. Genetic testing in severe aplastic anemia is required for optimal hematopoietic cell transplant outcomes. Blood. 2022.