Air Pollution, Medicinal Herbs Linked to Lung Cancer Mutagenesis in Never Smokers
, by Jennifer K. Loukissas, M.P.P.
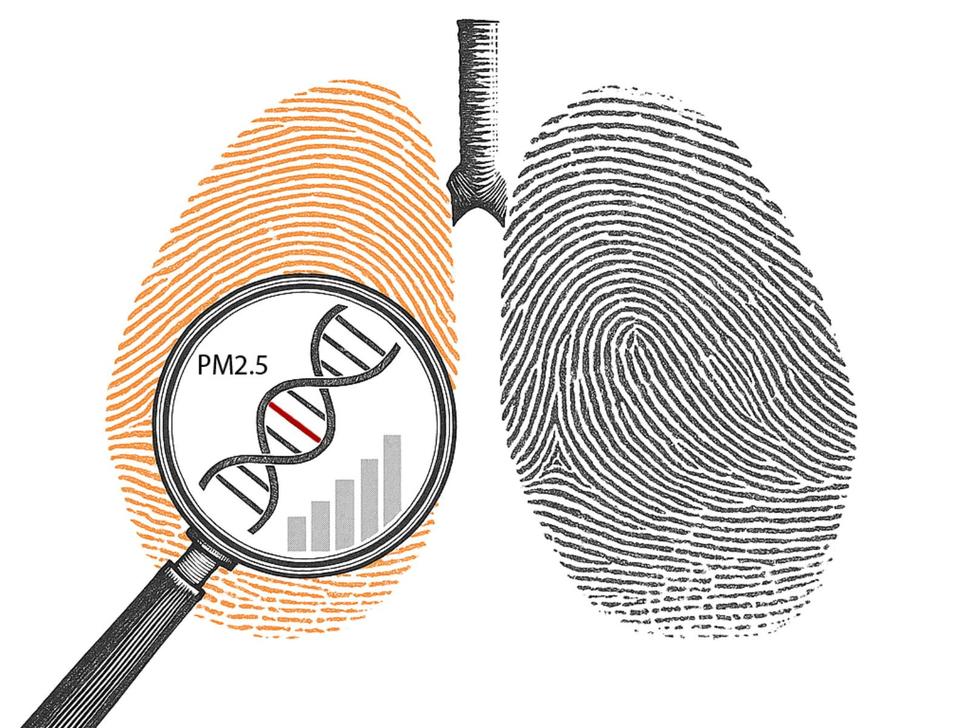
In the largest-ever whole-genome analysis of lung cancer in individuals who have never smoked, researchers at the National Cancer Institute and the University of California, San Diego, found exposure to fine particulate matter (PM2.5) air pollution was strongly associated with increased cancer-driving and cancer-promoting mutations through distinct biological pathways. The findings were published in the journal Nature on July 2, 2025.
The study team, led by Maria Teresa Landi, M.D., Ph.D., senior investigator, and Tongwu Zhang, Ph.D., Earl Stadtman Investigator, analyzed lung tumors from 871 never-smoker patients across 28 geographic locations worldwide as part of the Sherlock-Lung study. In the tumors of never-smoker lung cancer patients, they observed changes in the TP53 gene, and mutational signatures previously associated with tobacco smoking: Single Base Substitution (SBS) 4 and a mutation associated with age at diagnosis and cell division, SBS5. They also observed a dose-response relationship between air pollution and shorter telomeres.
Interestingly, while exposure to secondhand smoke was associated with slightly higher mutation burdens and shorter telomeres, compared to tumors in patients who were not exposed, the researchers did not find evidence that secondhand smoke increased cancer-driving mutations or mutational signatures. This suggests secondhand smoke has relatively low mutagenicity compared to air pollution and certainly compared to active tobacco smoking.
The origin of the most prevalent signature—SBS40—is unknown.
The SBS22a signature, which is associated with exposure to aristolochic acid, a compound found in medicinal plants, was present almost exclusively in tumors from patients in Taiwan. The route of exposure is likely medicinal use of herbs containing this compound. This is the first time this signature has been seen in lung cancer; it was previously found in other cancer types, including liver, kidney, and bladder cancer.
Prior genomic studies of lung cancer focused on tobacco smokers, leaving a significant gap in our understanding of how lung cancer develops in people who have never used tobacco. The aim was to uncover the mechanisms through which tissues acquire cancer-causing or cancer-promoting mutations following environmental exposures or endogenous processes. This information is critical in order to better understand the primary drivers of lung cancer in this population—who represent up to 25% of all lung cancer cases globally.
By examining the genetic mutations across different lung cancer subtypes, geographic regions, and environmental exposures, the researchers illuminated previously hidden drivers of lung cancer in never smokers. They hope this work will pave the way for prevention strategies for never-smokers.
This study builds on the 2021 findings from Sherlock-Lung: NIH Study Illuminates Origins of Lung Cancer in Never Smokers.
Reference
Díaz-Gay, M and Zhang T et al. The mutagenic forces shaping the genomic landscape of lung cancer in never smokers. Nature. 2025.