New Guidelines for Cervical Screening and Management Based on DCEG Research
, by Jennifer K. Loukissas, M.P.P.
For decades, researchers in the Division of Cancer Epidemiology and Genetics (DCEG) have studied the etiology of cervical cancer as well as the most efficient and effective means of prevention. Their work has provided the basis for clinical practice, both screening in the U.S. and worldwide, and clinical management of abnormal screening results in the U.S.
In the last 18 months, health organizations have published three major updates to those guidelines to reflect the latest scientific evidence in support of cervical cancer prevention. DCEG research on cervical cancer prevention through screening and management is conducted by a team of researchers in the Clinical Genetics Branch (CGB), Clinical Epidemiology Unit, led by Nicolas Wentzensen, M.D., Ph.D., M.S., Deputy Chief and senior investigator, and Mark Schiffman M.D., M.P.H., senior investigator. Below is a summary of those guidelines and the contributions of experts across.
U.S. Screening for Cervical Precancer: Recommendations from the American Cancer Society
In the summer of 2020, the American Cancer Society (ACS) released updated screening guidelines, prioritizing HPV testing as the most effective means to detect persistent HPV infection, the causal factor of cervical precancer; the guidelines were developed with input from DCEG investigators. Read a Q&A with Dr. Wentzensen on the NCI Cancer Currents blog to learn about the guidelines and the contributions of DCEG staff.
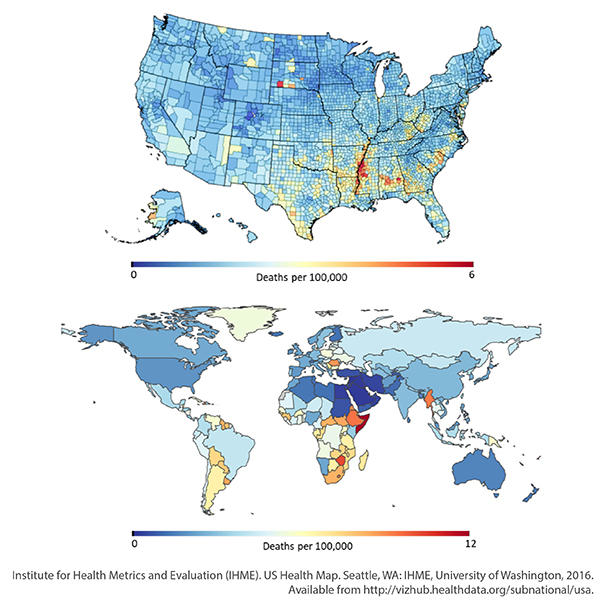
Approaches for Screening Worldwide, Including Low-resource Settings: Guidelines from the World Health Organization
In July 2021, the World Health Organization (WHO) released updated guidelines for the screening, management, and treatment of cervical cancers and precursors worldwide. Dr. Wentzensen and Julia C. Gage, Ph.D., M.P.H., staff scientist, served on the Guidelines Development Task Group and Dr. Schiffman on the External Review Group. Dr. Wentzensen also served on the Evidence Gathering Task Group.
While the WHO guidelines parallel recommendation from the ACS for primary HPV testing, they also outline a wider range of screening approaches and intervals serve populations across very different settings.
Clinical Management of Abnormal Screening Results
In April 2020, a consensus committee of cervical cancer experts from across the U.S. published a landmark set of recommendations for management of abnormal screening results, known as the 2019 ASCCP Risk-Based Management Consensus Guidelines. The guidelines are presented in a series of eight papers in the Journal of Lower Genital Tract Diseases and are available free on the web and as a downloadable application for smartphones.
The 2019 Consensus Guidelines are based on several fundamental concepts: management is based on risk, not individual test results; type and duration of HPV infection matter (the longer an HPV infection has been present, the higher the risk of pre-cancer and cancer); and screening history matters (the same current test results may yield different management recommendations depending on the history of recent past test results). The resulting shift in clinical practice will reduce unnecessary screening and interventions while improving detection of precancerous lesions. Read the main paper describing the guidelines and the introductory paper, which gives a summary overview.
DCEG Participants on Working Groups
- Dr. Schiffman, Steering Committee (co-chair)
- Dr. Wentzensen, New Technologies (co-chair)
- Dr. Megan Clarke, New Technologies
- Dr. Philip Castle, Surveillance (co-chair)
- Dr. Li Cheung, Risk Modeling and Statistical Analysis
- Dr. Didem Egemen, Risk Modeling and Statistical Analysis
- Dr. Maria De Marco, Co-factors Working Group
- Ms. Jennifer Loukissas, Communications (co-chair)
The Guidelines Committee followed a two-year process with 19 participating organizations that included federal agencies, medical professional societies, and—for the first time—patient advocacy groups. Dr. Schiffman co-chaired the steering committee and many DCEG experts played crucial roles on both the steering committee and on all seven of the working groups, advising on the interpretation of research data, risk modeling and statistical analysis, assay development, and testing, and health communications. See a full list of participants and roles in the box to the right.
Enduring Guidelines for Screening and Clinical Management
The shift to risk-based guidelines and clinical action thresholds allows for regular evaluation of new tests and approaches against existing thresholds, instead of developing new algorithms for each test, a more rapid and flexible process, compared to classic interim guidance and consensus conferences. DCEG and the members of the consensus committee coined this “living guidelines” approach the “Enduring Consensus Cervical Cancer Screening and Management Guidelines,” a system to ensure clinical practice keeps pace with scientific research. Central to the mission of the Enduring Guidelines is to increase targeted cancer prevention for high-risk individuals and decrease unnecessary invasive procedures in low-risk individuals and reduce health disparities. Dr. Wentzensen co-leads this multi-institutional effort.