Over the last three decades, the number of computed tomography (CT) examinations conducted annually has grown exponentially such that CT imaging currently represents about a quarter of the collective effective radiation dose received by the U.S. population. To address this public health concern, it is important to have tools to assess and monitor radiation exposures from CT scans. NCICT, the National Cancer Institute dosimetry system for Computed Tomography1-2 is a comprehensive cutting-edge CT organ dose calculator.
Robust Science
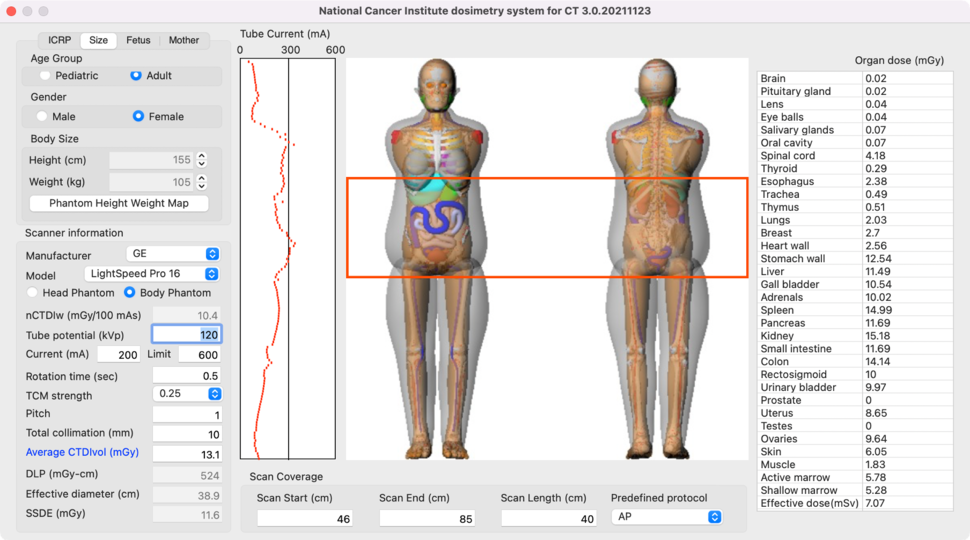
The program provides absorbed doses to major radiosensitive organs and tissues calculated using the characteristics of patients and CT scan parameters. NCICT combines several cutting-edge technologies, including a library of advanced computational human phantoms, the detailed simulation of x-rays from a reference CT scanner, and a user-friendly graphical interface. The simulated dose results for pediatric and adult phantoms have been rigorously validated through comparison with experimental measurements conducted using physical anthropomorphic phantoms combined with dosimeters3-5.
State-of-the-art Phantoms
NCICT incorporates a state-of-the-art library of phantoms that represent just about any patient, including the International Commission on Radiological Protection (ICRP) reference pediatric and adult phantom series, a library of 370 pediatric and adult male and female phantoms at various heights and weights, and eight pregnant phantoms containing detailed fetus models at various gestations6.
Hassle-free Installation
NCICT is a standalone software that runs on a personal computer. Users do not need an internet connection to upload sensitive patient data to a central server. NCICT uses a comprehensive pre-calculated dose database, so the program does not use up many computing resources on a user's computer. NCICT is available for multiple platforms, including Windows, Mac, and LINUX.
Versatile Dose Calculation Modes
NCICT features two computation modes: Graphical User Interface (GUI) mode and Batch Calculation mode. The GUI mode allows the user to enter interactively patient and CT scanner data for rapid organ dose calculations. The Batch Calculation mode is also available to compute organ doses for a large number of patients by importing a set of parameters from a formatted text file. The Batch Calculation mode also runs by text command, making it easy to connect NCICT with existing databases.
Extensively Tested
NCICT was rigorously tested by over 200 beta users whose feedback was incorporated into several revisions. The software has been used by hundreds of users worldwide and has resulted in many research publications.
How to Access This Resource
Non-Commercial Research Use
There is no charge to use these resources for non-commercial research purposes. Please click Software Transfer Agreement form, fill out the form in your web browser*, save it to your computer, then obtain the signatures and submit it to Dr. Choonsik Lee.
*Browsers tested with the form: Safari, Microsoft Edge, Google Chrome, and Firefox.
Commercial Use
Contact Dr. Kevin Chang of the NCI Technology Transfer Center to discuss accessing the free trial version and the licensing process for commercial use.