Overview
Radiotherapy is routinely used to treat cancer, including pediatric malignancies. This approach is often curative. However, radiotherapy is known to cause considerable morbidity and elevate risks for second cancers.
New modalities, such as proton beam therapy, have been developed to reduce radiation dose to surrounding healthy tissue and, consequently, the risk of developing cancer at those sites. The magnitude of the purported reduction in risk of second cancers remains uncertain. No randomized clinical trials comparing the two radiotherapy types have been conducted in children, who are more susceptible to the late effects of radiation compared to adults. Observational studies on this topic, while generally reassuring, have had important methodological limitations. The Pediatric Proton and Photon Therapy Comparison Cohort aims to meet this need.
Findings from this study will inform clinical practice for pediatric cancer patients by providing the first large-scale systematic comparison of the risk of second cancers from proton compared to photon therapy.
Study Team
National Cancer Institute Study Team
Cari Kitahara, Ph.D., Lead Principal Investigator, Radiation Epidemiology Branch (REB)
Choonsik Lee, Ph.D., Principal Investigator, REB, and Head, Dosimetry Unit
Todd Gibson, Ph.D., Staff Scientist, REB
Matthew M. Mille, Ph.D., Staff Scientist, Dosimetry Unit
Jungwook Shin, Ph.D., Staff Scientist, Dosimetry Unit
Keith Griffin, Ph.D., M.S., Postdoctoral Fellow, Dosimetry Unit
Sergio Morato Rafet, Ph.D., Postdoctoral Fellow, Dosimetry Unit
Isabelle van der Velpen, M.D., Ph.D., Postdoctoral Fellow, REB
Caroline Esposito, B.A., Postbaccalaureate Fellow, Dosimetry Unit
Massachusetts General Hospital Coordinating Center & Study Team
Professor Torunn Yock, Principal Investigator
Ms. Sara Gallotto, Project Manager
Mr. Benjamin Bajaj, Biostatistician and Technical Manager
Other Collaborators
Professor Amy Berrington, Principal Investigator, The Institute of Cancer Research (London, United Kingdom)
Background & Purpose
Proton therapy has emerged as a preferred radiotherapy modality for some cancers because the physical properties of protons lower doses to surrounding normal tissues and therefore should reduce acute and late-term adverse effects. In 2010, there were 24 proton therapy centers operating around the world. By 2021, 99 centers were in operation, and another 60+ were under construction or in the planning phase. As a result, there have been rapid increases in the number of cancer patients treated with proton therapy, especially children. We are studying pediatric patients because they are more susceptible than adults to the late effects of radiation exposure.
A pattern of care survey of U.S. centers found that the percentage of pediatric radiotherapy patients treated with proton therapy doubled from 2012 to 2016 (Journy et al., 2019), with 15% receiving this therapy by 2016. Half of the patients were aged <10 years and 25% were aged <5 years. CNS tumors accounted for 50% of cases and sarcomas 25%. Proton therapy was the most common form of radiotherapy used for rhabdomyosarcoma, medulloblastoma, ependymoma, and Ewing sarcoma (>50%). Similarly steep increases were reported using data from the National Cancer Database for pediatric CNS malignancies (Odei et al., 2017; Weil et al., 2022).
Proton therapy, particularly pencil beam scanning, is expected to lower second cancer risks due to more targeted delivery of the radiation to the site of the first primary cancer.
The Pediatric Proton and Photon Therapy Comparison Cohort aims to determine the magnitude of the purported reduction in risk of second cancer for children receiving proton versus photon radiotherapy. These findings will help to inform the treatment and long-term management of pediatric cancer patients.
See all DCEG research in the Cancer Survivorship Research Unit, or on medical radiation and radiation dosimetry.
Study Design
The Pediatric Proton and Photon Therapy Comparison Cohort aims to include 10,000 proton and 10,000 photon therapy patients treated between 2007 – 2023 in the U.S. and Canada for pediatric central nervous system tumors, sarcomas, Hodgkin lymphoma or neuroblastoma—the pediatric tumors most frequently treated with protons. Patient, cancer, and treatment characteristics will be abstracted from existing medical records at participating institutions. The study will build upon the infrastructure of the existing Pediatric Proton/Photon Consortium Registry (PPCR).
| Participating Institution | Principal Investigator | Modality | Year Center Joined |
|---|---|---|---|
| University of Colorado, Denver | Sarah Milgrom, M.D. | Photons | 2020 |
| Children's Hospital Los Angeles | Kenneth Wong, M.D. | Photons | 2020 |
| University Health Network Toronto | Derek Tsang, M.D. | Photons | 2021 |
| Massachusetts General Hospital | Yorunn Yock, M.D. | Protons | 2021 |
| University of Florida | Daniel Indelicato, M.D. | Protons | 2021 |
| Mayo Clinic - Rochester | Anita Mahajan, M.D. | Protons/Photons | 2021 |
| Emory University | Bree Eaton, M.D. | Protons/Photons | 2021 |
| The Ohio State University | Joshua Palmer, M.D. | Photons | 2021 |
| University of Utah | Matthew Poppe, M.D. | Photons | 2021 |
| University of Pennsylvania/CHOP | Christine Hill-Kayser, M.D. | Protons/Photons | 2023 |
| MD Anderson Cancer Center | Arnold Paulino, M.D. | Protons | 2023 |
| California Protons Cancer Therapy Center | Iain MacEwan, M.D. | Protons | 2023 |
| Baylor University | Murali Chintagumpala, M.D. | Photons | 2023 |
| Chicago - Northwestern | John Kalapurakal | Protons | 2024 |
| Washington University in St. Louis | Stephanie Perkins | Protons/Photons | 2024 |
| Procure New Jersey | Jae Y. Lee | Protons | 2024 |
| Mayo Clinic - Arizona | Safia Ahmed | Protons | 2024 |
Radiation exposure assessment will be based on state-of-the-art dosimetry techniques facilitated by the collection of electronic radiotherapy records for all eligible patients. Second primary cancers and mortality will be ascertained by linkage to cancer and mortality registries. The primary analysis will examine second cancer risk following proton compared to photon therapy, adjusting for potential confounders and accounting for competing risks.
The study is expected to continue for decades in order to capture the range of the late effects that may be associated with these therapies.
Select Publications
Select Publications
Cohort Design and Methods
Berrington de González A, et al. The Pediatric Proton and Photon Therapy Comparison Cohort: Study design for a multicenter retrospective cohort to investigate subsequent cancers after pediatric radiation therapy. Advances in Radiation Oncology 2023.
Commentary on the need for a large-scale, international collaborative study
Berrington de González A, et al. A clarion call for large-scale collaborative studies of pediatric proton therapy. Int J Radiat Oncol Biol Phys 2017.
Dosimetry Methods
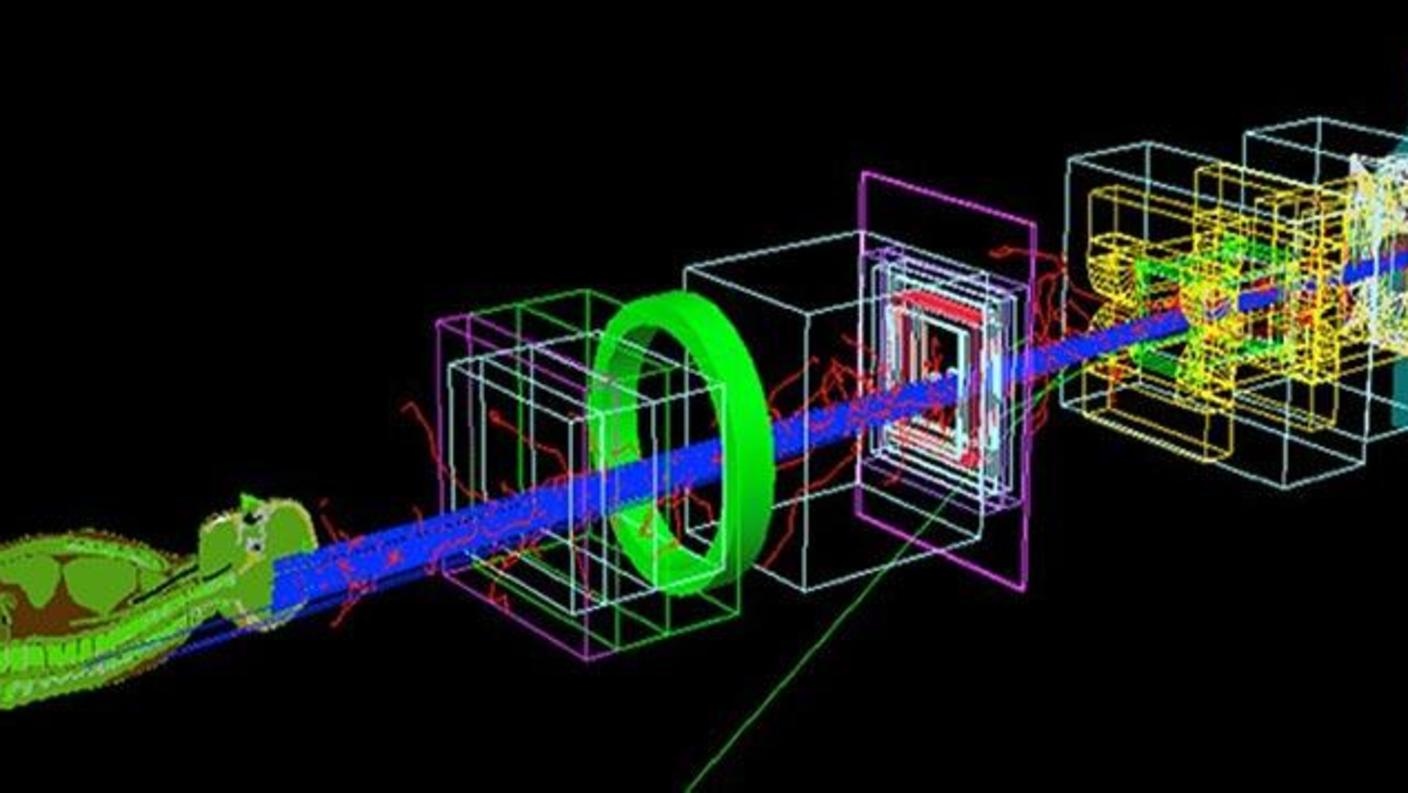
Yeom YS, et al. A Monte Carlo model for organ dose reconstruction of patients in pencil beam scanning (PBS) proton therapy for epidemiologic studies of late effects. J Radiol Prot 2020.
Yeom YS, et al. A dose voxel kernel method for rapid reconstruction of out-of-field neutron dose of patients in pencil beam scanning (PBS) proton therapy. Phys Med Biol 2020.
Griffin K, et al. Comparison of out-of-field normal tissue dose estimates for pencil beam scanning proton therapy. Biomed Phys Eng Express 2023.
Data Sharing
De-identified data will be made available upon completion of data collection and publication of the primary analysis manuscript, in accordance with the NIG Data Sharing Policy and policies of participating institutions.
Funding
Funding for the data collection and management of this study has been provided by the NCI’s Childhood Cancer Data Initiative (CCDI) and the Intramural Research Program of the National Cancer Institute.